The Road to Interoperability Has Led Healthcare to the FHIR Standard
FHIR (pronounced “fire”) might be the hottest (sorry) topic in healthcare technology. EHRs have adopted it as the standard for sharing data with other systems and healthcare information exchanges (HIEs).
So what is FHIR, and what does the standard and technology promise for healthcare? This article breaks it down:
- What is the FHIR Standard?
- How Does FHIR Work?
- Who’s on FHIR?
- What is SMART on FHIR?
- What Can the FHIR Standard Do for Healthcare?
What is FHIR?
Fast Healthcare Interoperability Resources (FHIR) is an advanced, open-source standard for healthcare information exchange across EMRs and other systems.
Health Level Seven International, the standards bearers for healthcare interoperability, first released FHIR in 2014, building on decades of work with the HL7 standard. It quickly emerged as the most powerful and elegant way yet for healthcare systems to have meaningful conversations with each other.
Most EHRs have embraced these API standards for sharing data. Big players like Apple also rapidly adopted the FHIR interface standards and protocols, additionally boosting its momentum throughout healthcare. The 21st Century Cures Act and final rules from the Centers for Medicare Services (CMS) have since mandated the adoption of the standards by most every healthcare organization. Payers in particular have pressure to adopt the standard and expand patient access to their health data by connecting and sharing with other systems.
If you’re in healthcare, you’re playing with FHIR. (Sorry again.)
How Does FHIR Work?
FHIR sets a structure for extending and customizing resources that can be universally read by any system, regardless of their origin. The standard uses APIs to smoothly integrate various apps into a central operating system, simplifying data flow within the provider’s workflow.
First, let’s take a step back: What is a healthcare data interface?
A data interface is software that lets two systems or applications talk to each other and share data. We most often refer to it as an application programming interface (API).
So, let’s think of data as shapes. In one healthcare system, a particular data element (say, a provider code) is a circle. A second healthcare system identifies the provider code as a rectangle.
An API sits between the two systems and allows them to exchange data and recognize both the circle and the rectangle as the same type of provider code.
That’s an extremely basic example. For healthcare, we can quickly see how complex such data exchange can get. Dozens of EHRs and healthcare information and technology systems define and recognize hundreds of data types and elements differently.
As EHR adoption expanded in the late 1970s and through the 1980s, “interoperability” was a chaotic landscape with hundreds of custom system-to-system interfaces built by vendors. There was no single, common standard that defined the data sets, technologies, and API structure for health data exchange.
In 1987, HL7 emerged as the first major standard for healthcare data exchange designed to control that chaos. HL7 and its subsequent versions led healthcare forward in big steps to enable different EHRs and health systems to share data with a common interface standard.
But HL7 has some limitations. Older socket-based, SOAP, and XML protocols have a steep learning curve for developers. Mapping every single piece of data can limit the context and understanding when passed to another system, diminishing its usefulness.
And HL7 only works with structured data, with a set data model organized in fields with specific formats and meanings. Think of a healthcare database or spreadsheet with discrete, rigidly defined fields for things like patient name, lab result, prescription name and quantity, and insurance and financial information.
Unstructured data—things like scanned images, handwritten doctor notes, and PDF files—comprise 80 percent of all healthcare data. Healthcare cannot achieve completely meaningful interoperability without it.
How Does FHIR Support Patients and Providers?
The healthcare IoT sector is growing fast, but tools to connect PGHD with provider workflows are lacking. FHIR uses web APIs for patients and physicians to easily access and share health info from anywhere, aligning healthcare with Internet-based experiences.
Moreover, FHIR offers a chance to blend Electronic Health Records (EHR) with diverse PGHD sources such as wearables and remote patient monitoring (RPM), streamlining access for healthcare providers to leverage and respond to invaluable insights. Tailored apps developed on a FHIR platform could analyze PGHD to offer users a concise overview of pertinent trends in chronic disease management or patient well-being.
Patients also get a comprehensive view of their data through FHIR. For example, Apple’s Health app on iOS leverages FHIR to aggregate patient data from EHRs and healthcare facilities. Healthcare professionals, therefore, can customize tools according to patients’ demands to boost clinical decision-making and advance precision medicine.
For healthcare providers, FHIR enables them to connect with third-party apps from their EHR, breaking free from system constraints. Adhering to FHIR standards allows providers to develop apps with vendors more efficiently and economically, ensuring data consistency across all sources.
The Evolutionary Difference
FHIR, first released by Health Level Seven International in 2014, became the next-generation HL7 data exchange standard. We can look at how the standard works in the context of how it expands the capabilities of HL7:

- Solves Unstructured Data Exchange: The FHIR standard allows systems to share structured and unstructured data, closing the most critical interoperability gap and eliminating onerous manual input and communications. It also vastly expands the universe of health data that systems can exchange.
- Helps Build Interfaces Faster and Easier: Built using HL7, the FHIR standard embraces more modern API technology, including the RESTful protocol, and a choice of JSON, XML, or RDF for representing data. Developers have more experience with these advanced tools, making the standards easier to learn and APIs easier to develop and implement.
- Introduces Resources to Make Better, More Intuitive Sense of Data: The FHIR standard introduced the concept of resources to health data exchange. Resources are data categories that represent common healthcare concepts and components, such as patients, lab results, insurance claims, appointments, and more. The standard identifies 145 resources in all. This makes interfaces much more flexible and development more intuitive, while also making it easier for other systems to recognize, organize, and use the data.

Does FHIR Advance Semantic Interoperability?
HIMSS says that interoperability “describes the extent to which systems and devices can exchange data and interpret that shared data. For two systems to be interoperable, they must be able to exchange data and subsequently present that data such that it can be understood by a user.”
HIMSS defines three technical tiers of interoperability: Foundational, structural, and semantic.
- Foundational Interoperability: One healthcare system can send data to another. The other system might not know what the data is or means, but it can confirm receipt.
- Structural Interoperability: One healthcare system can send data to another system that understands what the data is and what it’s for.
- Semantic Interoperability: Healthcare systems can exchange, interpret, and actively use the data. This is what everyone in healthcare wants to achieve, sharing patient data across all systems that looks the same to patients, doctors, technicians, payers, accountants, and everyone involved in the quality patient journey.
While healthcare organizations have made great progress in integration, many still operate in the first two tiers of interoperability.
FHIR has accelerated healthcare’s journey to faster, more intelligent, and more useful semantic data sharing. But healthcare technologists caution that the standard cannot yet get to full semantic interoperability because of variations in collecting, coding, and processing data. Other active technology efforts are under way to add the next layer of semantic intelligence and exchange to FHIR messages and other data sets.
New technologies and iterations of the standards will keep healthcare moving toward true interoperability, just as FHIR iterated huge progress in data exchanges from previous HL7 versions.
Who’s in for the change?
EHRs: The good news: All major EHRs have established FHIR-based APIs to share and exchange clinical data, which was one of the keys to building consensus and momentum for the standard. These EHRs include EPIC, Cerner, Allscripts, athenahealth, CPSI , eClinicalWorks, MEDHOST, MEDITECH, and NextGen. Those players alone cover 83 percent of hospitals and 53 percent of clinicians. The less-good news: Wider adoption and connection to these interfaces remains low and slow. But interoperability all starts with the EHR, so at least the FHIR foundation is in place.

The Game Changers: Apple quickly adopted SMART on FHIR to connect with EHRs and provide consumers with their medical records. This early endorsement by a giant, recognized leader in technology innovation and its tens of millions of users represented a breakthrough in establishing FHIR as the clear standard for interoperability moving forward. Walmart, Google, Amazon, and Microsoft are all pursuing FHIR-based solutions and stand to set the course for patient-focused capabilities of free health data exchange.
Payers: The 21st Century Cures Act mandates the adoption of FHIR standards for data exchange among healthcare systems and calls for three distinct payer-focused APIs for patient access, provider directories, and payer-to-payer communication. Payers face imminent compliance deadlines in 2022 for them to publish APIs that connect patients with their health information.
Providers: Adoption is high but limited, mostly driven by FHIR APIs provided by EHRs for hospitals and practices. Hospitals have still been slow to adopt the standard to improve other areas, including obvious ones like patient access and consumer service. The big players like Apple and Walmart might run right past them in defining the connected patient experience, essentially locking providers out of their own digital front door.
What is SMART on FHIR?
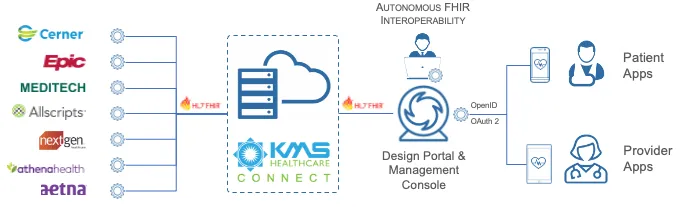
SMART on FHIR is a systematic way for an application to securely request authorization to access data, then retrieve and use it. SMART on FHIR offers a health application interface built on open standards such as HL7’s FHIR, OAuth2, and OpenID Connect.
A New England Journal of Medicine article first suggested building a universal API to define how patient-facing apps could connect and communicate with EHR systems. The Harvard Medical School and Boston Children’s Hospital collaborated to launch SMART (Substitutable Medical Applications and Reusable Technologies). The mission: Let healthcare IT technology developers build a single app that works with any health information system.
SMART on FHIR combines SMART open-source tools with the FHIR API. SMART on FHIR apps let providers, payers, and patients view patient records, monitor cardiovascular health, schedule services, and much more. They pull in all the data they need from any EHR system, whether it’s Epic, Cerner, AllScripts, athenahealth, or another vendor.
SMART defines how third-party apps will work with EHRs, which specific users are connected, and what patient data they are retrieving. It also publishes protocols for client authentication and authorization to connect to FHIR servers.
The 21st Century Cures Act and Centers for Medicare Services rules mandate SMART certification. So SMART on FHIR app development will be a big, lasting part of healthcare’s technology future.
What Can FHIR Do for Healthcare?
By getting all healthcare systems to speak and understand the same language, the FHIR standard can:
- Make healthcare data exchange faster, more efficient, more accurate, more useful than ever before
- Improve clinical point-of-care decisions and care coordination
- Give consumers and patients more access to their health information from all systems
- Amplify financial performance by adding precision and speed to the revenue cycle
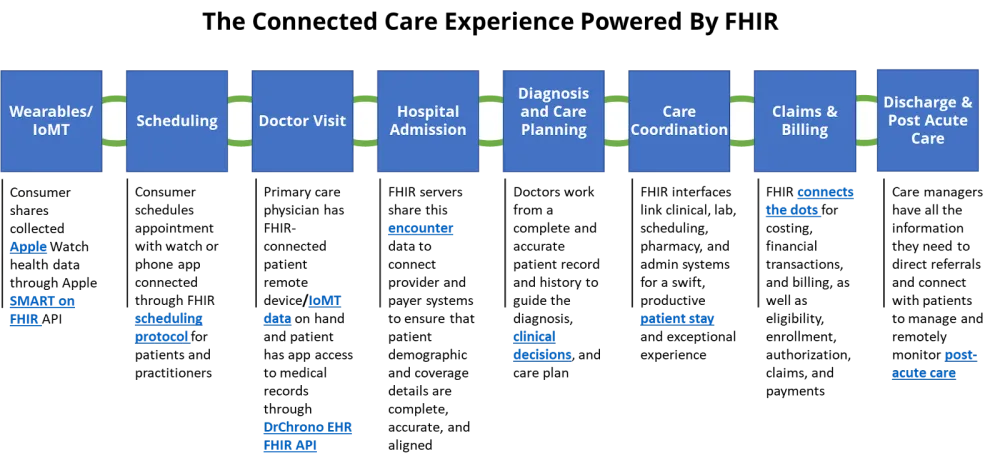
This list of potential and real benefits for healthcare goes on and on. They add up to a Connected Care Experience for patients, doctors, nurses, care coordinators, lab techs, claims processors and billers, discharge planners, and everyone involved in the care journey. Let’s look at that vision:
How It Powers the Connected Care Experience
What’s Next in Store?
The promise and possibilities for the FHIR standard in healthcare have few bounds. Every health IT company, provider, and payer must have clear plans for interoperability to consume and use patient data meaningfully in their workflows.
Software companies, providers, and payers must seek the fastest, most reliable path to connect their systems and share data using the standard.
But building a FHIR interoperability strategy and interfaces within your own organization remains complex. Healthcare IT leaders acknowledge that they still have a lot to learn about where and how to take smart advantage of the standard.