Remote patient monitoring (RPM) is more cost-effective than standard care in treating chronic disease.
Chronic diseases have far-reaching impacts on society, placing a significant economic strain on healthcare systems through ongoing medical expenses and reduced productivity due to illness and fatalities. According to the CDC, 90% of the nation’s healthcare costs can be attributed to individuals with chronic diseases and mental health conditions.
The potential of remote patient monitoring to predict worsening conditions benefits both patients and healthcare providers. Besides financial considerations, several studies demonstrate that integrating RPM also leads to positive patient treatment outcomes.
This blog examines the applications of RPM systems in Chronic Care Management (CCM), providing practical use cases of this advancing technology and a comparative analysis of how an innovative RPM solution operates.
Overview of Remote Patient Monitoring

What is Remote Patient Monitoring?
Remote patient monitoring (RPM) utilizes digital technologies that collect health data from patients in distant locations and transmit it to healthcare providers for analysis and treatment. This real-time data exchange enables continuous patient monitoring outside traditional healthcare settings. Implementing RPM fosters a personalized healthcare approach, allowing for timely interventions and tailored care for patients across various locations.
Integrated Remote Patient Monitoring System Overview
The system starts with medical equipment patients utilize in RPM setups to gather essential health data. These tools can monitor vital signs like blood pressure, heart rate, glucose levels, and oxygen saturation to assess the patient’s health comprehensively.
The data collected from these devices is then wirelessly transmitted from the system’s second component, typically via Bluetooth or WiFi, to the patient’s smartphone, tablet, or computer. This wireless transmission marks a significant technological advancement, instantly reducing manual data entry and ensuring accurate, up-to-date health records.
The securely transferred information is then directed to healthcare providers through robust cloud systems, enabling remote monitoring of patient health, immediate notifications of critical changes, and informed decisions on treatment and care. This aspect of RPM significantly enhances healthcare responsiveness and efficiency.
The RPM system’s final component involves linking with a patient’s Electronic Health Records (EHR). A comprehensive, long-term view of the patient’s health history is maintained by directly inputting RPM data into the EHR system. This integration supports consistent care and improves healthcare decision-making by offering a detailed historical context.
Read more: Key Technology Considerations for Successful Remote Patient Monitoring Projects
What is Chronic Disease Management?
Chronic care management entails continuous support for enduring conditions such as mental health problems, diabetes, heart disease, Alzheimer’s, or any condition persisting for six months or longer. With six out of 10 Americans facing chronic diseases, effective collaboration with their healthcare provider is crucial for improving symptom control and overall well-being within the healthcare framework. RPM is the intermediary that connects patients with chronic ailments to healthcare professionals, ensuring they receive convenient and appropriate care.
Benefits of Remote Patient Monitoring in Chronic Disease Management

Remote patient monitoring complements chronic disease management by enabling healthcare professionals to remotely and instantly monitor patients. This synchronization offers various benefits to the patients and healthcare institutions as well, including:
- Frequent monitoring
- Right-time intervention
- Improve patient experience
- Reduce incurred costs
- Increase profits margin
1. Frequent Monitoring
CCM involves monthly follow-ups with patients to review their treatment plans, whereas RPM eliminates the need for patients to remember symptoms from the previous month. Eliminating patient input here can reduce lag time and diagnosis errors. By connecting the “demand” with the right “features,” RPM enables healthcare practitioners to monitor patient vitals and effectively assess the treatment plan’s impact on biometrics.
For example, patients with hypertension who aim for a specific blood pressure level can analyze their progress over time using health monitoring devices. Blood pressure monitors and glucose meters measure goal achievement. Furthermore, RPM boosts the frequency of patient health monitoring by facilitating daily or weekly data gathering.
2. Right-time Intervention
By increasing monitoring frequency, healthcare professionals can promptly detect changes in patient health and step in before conditions worsen. For example, RPM offers high sensitivity (98.7%) and specificity (99.3%) in identifying blood sugar level spikes. These featured updates enable timely alerts to healthcare providers, prompting adjustments to the patient’s medication or treatment plan.
3. Improve Patient Experience
RPM supports CCM by providing healthcare providers with a comprehensive view of their patients’ well-being, enabling personalized care based on individual needs. Specifically, this approach enhances patient engagement by encouraging patients to take a proactive role in their healthcare journey. With real-time health information at their fingertips, patients are more engaged in managing their health conditions, leading to improved adherence to treatment plans.
4. Reduce Incurred Costs
Healthcare providers can reduce healthcare costs significantly by integrating CCM with RPM. This strategic combination plays a vital role in minimizing hospital admissions, emergency room visits, and the need for costly medical interventions. By leveraging CCM and RPM together, healthcare organizations can proactively monitor and manage patients’ health conditions, improving outcomes and reducing financial burdens on patients and the healthcare system.
5. Increase Profit Margins
RPM can significantly boost profit margins for healthcare organizations by reducing operational costs. Unlike traditional in-person visits that require supplies like gloves and sanitizers for each patient, RPM minimizes the need for physical resources, resulting in cost savings for clinics. This approach increases appointment numbers and reduces resource consumption, proving to be an effective strategy for improving the profit-to-loss ratio in healthcare settings.
Due to updated CPT codes in 2020, Medicare, Medicaid, and various private payers in 34 states have started covering remote monitoring. Compensation is in place for providers to set up and train patients on RPM. Healthcare providers also receive a fixed monthly fee for overseeing health monitoring devices and recording readings, with RPM payments reflecting clinical staff’s monthly time dedicated to patient care management.
Ultimately, RPM enables practices of all sizes and specialties to establish consistent income streams, potentially generating $1,764 per patient annually for healthcare institutions.
Notable Chronic Care Use Cases Of RPM

Remote patient monitoring has become a valuable tool for improving patient outcomes and care management. However, the true power of RPM also lies in its ability to address specific chronic conditions. RPM can effectively manage chronic illnesses, empower patients, and improve their quality of life. Mainly, RPM treatment has been deployed for patients battling:
- Diabetes
- Hypertension
- Respiratory conditions
1. Diabetes
Substantial evidence supports using RPM to improve diabetes management, prompting healthcare providers to incorporate this approach into their services. Connected glucose monitors play a crucial role by tracking blood sugar levels, providing trend insights, and alerting providers to potential issues, enabling timely treatment adjustments.
A 2019 study demonstrated that patients engaging more frequently in remote monitoring achieved lower hemoglobin A1c levels, indicating improved diabetes control. Moreover, RPM tools are beneficial not only for type 2 diabetes patients but also for young children with type 1 diabetes. Research from Stanford Children’s Health revealed that 53% of children using continuous glucose monitors reached the care goal of maintaining an A1c below 7%.
2. Hypertension
Numerous research studies show that RPM can effectively manage and reduce high blood pressure. Specifically, individuals with hypertension can benefit from continuous blood pressure monitoring through RPM. This proactive approach allows healthcare professionals to promptly intervene by adjusting medications or recommending lifestyle changes to maintain healthy blood pressure levels.
A study found that about 81% of hypertension patients participating in a home-based BP monitoring program reached their blood pressure goals in around seven weeks. Home-based BP measurements were also more reliable and accurate than those taken in clinical settings or kiosks. As a result, many healthcare providers have incorporated RPM into their strategies for managing hypertension.
3. Respiratory Conditions
RPM can benefit patients with respiratory conditions like chronic obstructive pulmonary disease (COPD) or asthma. Connected devices can track lung function, detect changes in breathing patterns, and assist in optimizing medication management.
Research has proved that RPM could improve the accuracy of COPD diagnosis and treatment. Moreover, patients are receptive to using telemonitoring systems for at-home pulmonary rehabilitation. In a scientific survey, 98% of participants found the system easy to use and were eager to utilize it throughout their pulmonary rehab program.
Real-World Application of Remote Patient Monitoring from Experts’ View
Recognizing the vast advances and practical applications of RPM, our experts at KMS Healthcare have made further efforts to deploy RPM solutions more broadly. Our Innovative Lab aims to provide an effective solution for capturing and relaying critical health data from patients through innovative and scalable experiments.
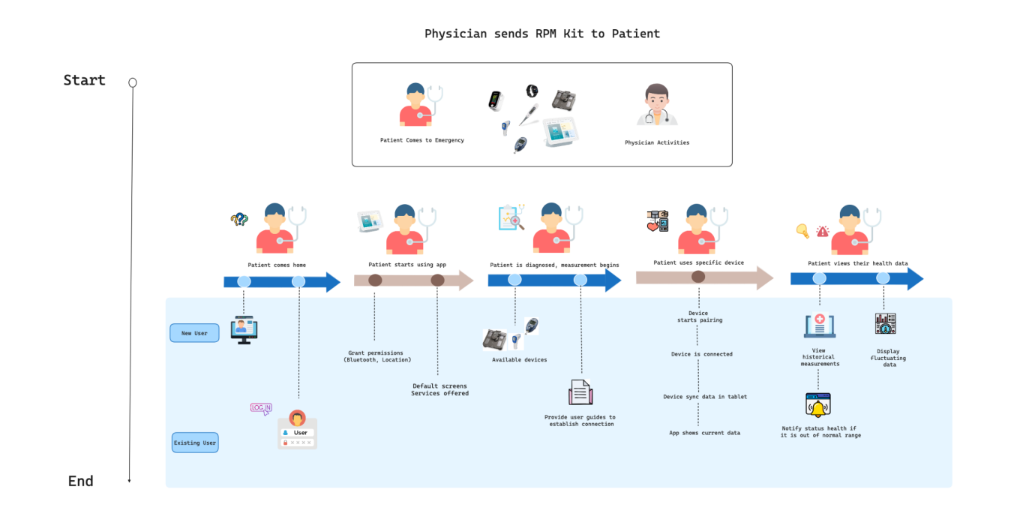
In addition to the primary RPM tracking mechanism (Figure 1), what sets the RPM solution apart is the architecture of the multi-tenant RPM SaaS system, which is designed to provide a scalable and secure platform for our users and health providers (Figure 2).
The application layer oversees user tasks, data processing, and workflows through APIs and microservices. The database layer processes data storage and management, while the data streaming layer facilitates real-time processing of RPM device data.
The integration layer also enables external system integration. The infrastructure layer, supported by cloud providers, virtual machines, and containers, ensures reliable hosting and scalability. Security and compliance protocols are maintained throughout the architecture to protect user data and meet industry regulations. Bluetooth Low Energy (BLE) is also utilized for device connectivity to ensure energy efficiency and low-latency communication.
Make Remote Patient Monitoring Your Next Innovation!
RPM is already delivering on its potential and promises in the field. However, CCM is a continuous journey that evolves, requiring frequent RPM customizations according to patients’ conditions. In addition to the core technologies within the system, healthcare organizations need expert advisory services to navigate these modifications and improve the CCM process.
With 15 years of experience, KMS Healthcare is your reliable partner in this field. Beyond consistently updating RPM systems for emerging developments, KMS Healthcare’s experts offer healthcare institutions valuable guidance and strategies for effective RPM implementation.

Seize the opportunity to collaborate with a partner delivering top-notch technology services and expert support in the growing field of RPM. Schedule a consultation today!