In recent years, technological advancements have driven digital transformations across industries, including healthcare. Once characterized by paper records and manual data entry, healthcare now features telehealth, wearable health trackers, cloud storage, and strong cybersecurity measures.
However, not all transformations are smooth. Post-COVID-19, only 30% of organizations reported successful digital transformation projects, with legacy systems being a key obstacle. According to a 2021 HIMSS survey, 73% of healthcare providers still rely on outdated systems. Additionally, a 2022 Mulesoft report found that organizations use an average of 976 unique applications, many likely legacy systems.
Legacy systems can hinder efficiency, data security, and patient care. In this blog, we’ll explore legacy systems, their impact on healthcare, and how to modernize them effectively.
What is a Legacy System in Healthcare?
A legacy system in healthcare refers to outdated software, technology, or processes that are no longer maintained, updated, or fully supported. These systems often struggle with interoperability, pose security risks, and require costly maintenance. They typically use outdated operating systems (e.g., Linux, Unix) or hardware platforms (e.g., old servers, networking equipment) and may be built with obsolete programming languages. This leads to integration challenges, data safety issues, and noncompliance with modern healthcare standards.
Common Reasons for Legacy Status:
- Vendor Discontinuation: The technology is at its end of life.
- Lack of Updates: No routine maintenance or updates from the vendor.
- Security Risks: No active monitoring for bugs or cybersecurity patches.
- Limited Scalability: The technology cannot accommodate growth.
- Operational Gaps: No qualified staff to operate or manage the system.
Examples of Legacy Systems in Healthcare:
- Electronic Health Record (EHR) Systems: Older EHRs often lack modern functionalities, interoperability, and intuitive interfaces.
- Hospital Information Systems (HIS): Legacy HIS may struggle with real-time data access and modern reporting.
- Laboratory Information Systems (LIS): Outdated LIS may have integration and data standardization issues.
- Picture Archiving and Communication Systems (PACS): Legacy PACS might not be compatible with modern imaging technologies.
- Radiology Information Systems (RIS): Older RIS may lack advanced scheduling and integration features.
- Telemedicine Systems: Legacy telemedicine systems often need upgrades for secure communication and efficient telehealth services.
- Claims Processing Systems: Outdated systems may not adapt well to modern billing rules and regulatory changes.
- Patient Engagement Systems: Early versions often lack the user-friendly features needed for active patient involvement.
The Risks of Legacy System in Healthcare
Relying on outdated legacy systems in healthcare poses real risks to security, efficiency, and patient care quality.
1. Security Risks
Legacy systems in healthcare often expose medical facilities to substantial cybersecurity risks due to outdated technology and inadequate security features. Many of these systems were developed without robust hardware and software mechanisms to defend against modern cyber threats, leaving healthcare providers vulnerable to potential attacks. The lack of advanced encryption, multi-factor authentication, and secure data handling practices can create significant security gaps.
When healthcare systems are not well-protected, medical facilities may face severe consequences, including patient confidentiality breaches, data loss, or unauthorized access to sensitive medical records. Such incidents can lead to legal penalties, damage to the healthcare provider’s reputation, and a loss of patient trust. Ultimately, cybersecurity vulnerabilities can negatively impact the quality of healthcare services and hinder the organization’s ability to provide safe and effective care.
2. High Maintenance Costs
Maintaining outdated healthcare systems can be a costly endeavor for medical institutions. Frequent repairs, software updates, and the need to hire specialized personnel to manage obsolete technologies can divert financial resources away from critical patient care initiatives. The high maintenance costs associated with legacy systems often hinder an organization’s ability to adopt modern healthcare solutions that improve efficiency and patient outcomes.
Modernizing legacy systems offers a strategic solution to reduce maintenance costs. Updated healthcare systems are more adaptable, scalable, and compatible with evolving technological standards. By transitioning to modern software infrastructure, healthcare facilities can allocate resources more effectively, supporting initiatives that benefit patient care and operational efficiency.
3. Inability to Adopt Advanced Technologies
Healthcare organizations that continue using legacy systems may struggle to adopt new technologies such as artificial intelligence, machine learning, and predictive analytics. These advanced solutions can significantly improve patient care, streamline workflows, and reduce operational costs. However, outdated systems often lack the integration capabilities to support these innovations.
Upgrading healthcare technology creates a foundation for adopting advanced tools and systems. Modernized systems offer greater flexibility and compatibility, helping healthcare providers stay competitive and deliver enhanced services.
4. Compromised Patient Safety
Outdated healthcare systems can pose serious risks to patient safety. When software lacks interoperability, healthcare providers may not have access to complete or accurate patient data, leading to misdiagnoses, treatment errors, and adverse events. Effective communication between healthcare systems ensures precise information exchange and coordinated patient care.
Legacy systems may also hinder clinical workflows, causing delays or inaccuracies in data transfers. These challenges increase the likelihood of medical errors, potentially compromising patient safety. Adopting updated technology improves data accuracy, communication, and clinical decision-making, leading to safer healthcare practices.
5. Compliance and Regulatory Hurdles
Compliance with healthcare regulations such as HIPAA, GDPR, and PIPEDA is crucial for protecting patient data and avoiding legal repercussions. Legacy systems often fall short of modern compliance standards due to outdated security features and limited adaptability to regulatory changes. This gap can expose healthcare organizations to data breaches, financial penalties, and reputational harm.
Modernizing legacy systems offers a practical solution to compliance challenges. Updated healthcare software incorporates advanced data protection protocols designed to meet current regulatory requirements, strengthening compliance and enhancing patient data security.
Addressing the risks of legacy systems is a critical step in supporting the digital transformation of healthcare organizations. Modern systems provide better security, reduce costs, and enable the adoption of innovative technologies that improve healthcare quality and efficiency.
Maintaining or Modernizing Legacy Systems: Pros and Cons
Whether to maintain or modernize legacy healthcare systems is a critical decision for healthcare organizations. Each approach offers distinct advantages, and the best choice depends on the organization’s specific needs, resources, and long-term goals.
Advantages of Maintaining Legacy Healthcare Systems
- Cost Efficiency: If current systems are performing well, maintaining them can avoid the high upfront costs associated with modernization.
- Operational Stability: Staff are already familiar with existing systems, minimizing the need for extensive training and reducing the risk of disruptions.
- System Compatibility: Legacy systems often work well with existing applications and infrastructure, avoiding integration challenges.
Advantages of Modernizing Legacy Healthcare Systems
- Enhanced Efficiency: Modern systems incorporate advanced technologies that streamline workflows, improve operational efficiency, and support interoperability.
- Advanced Security: Modernization introduces sophisticated security features that protect patient data and maintain compliance with healthcare regulations.
- Future-Proofing: Updated systems are more adaptable to emerging technologies, providing a solid foundation for organizational growth and innovation.
Ultimately, the decision to maintain or modernize should consider the system’s current performance, available resources, and the organization’s strategic objectives. While maintaining legacy systems can be beneficial in the short term, modernization is often necessary to meet evolving healthcare standards and ensure long-term success.
Comparison: Maintaining vs. Modernizing Legacy Healthcare Systems
| Criteria | Maintaining Legacy Healthcare System | Modernizing Legacy Healthcare System |
| Cost | Lower immediate costs with potential hidden expenses | Higher upfront costs with long-term financial benefits |
| Scalability | Limited ability to scale with organizational needs | Easily scalable to support growth and new technologies |
| Effectiveness | Familiarity for staff, reducing learning curves | Tailored to meet evolving business and clinical requirements |
| Security | Potential vulnerabilities due to outdated updates | Strong data protection and compliance with the latest regulations |
| Integration | Difficult to connect or work with other systems apps | Seamless integration for smooth data exchange and system interoperability |
While maintaining legacy systems may offer short-term stability and cost control, modernizing healthcare technology delivers significant scalability, security, and efficiency benefits. Organizations must weigh these factors carefully to make the best choice for their long-term goals and patient care standards.
Methods to Modernize Legacy Systems in Healthcare
Modernizing legacy systems in healthcare involves several strategies, each tailored to the specific needs of the organization and the state of its existing technology. Choosing the correct method can enhance system performance, improve scalability, and ensure compliance with evolving healthcare standards. Here are six practical approaches to modernizing legacy healthcare systems:
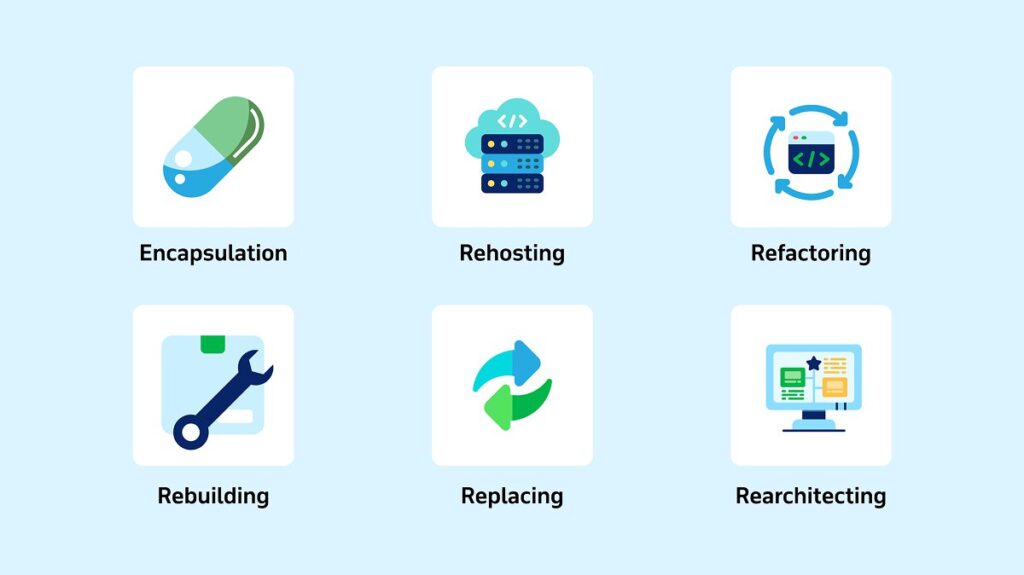
1. Encapsulation
Encapsulation involves wrapping legacy systems with modern interfaces or APIs, enabling newer applications to interact seamlessly with older systems. This approach is ideal when healthcare organizations want to maintain the core functionality of existing systems while enhancing integration capabilities. For instance, a hospital can introduce a modern electronic health record (EHR) system that communicates with older laboratory or billing systems through APIs, ensuring smooth data flow without altering the legacy codebase.
Encapsulation is particularly useful when a full-scale system overhaul is not feasible. It offers a cost-effective and time-efficient solution to enhance interoperability, allowing healthcare facilities to integrate new technologies gradually while avoiding significant disruptions to daily operations.
2. Rehosting
Rehosting, or ‘lift and shift,’ involves migrating legacy applications to new infrastructure or platforms, such as moving from on-premises servers to the cloud. This method does not require changes to the application code, making it a suitable choice for stable systems that could benefit from modern infrastructure capabilities.
Healthcare organizations often use rehosting to improve performance, reduce infrastructure costs, and enhance disaster recovery options. For example, rehosting a hospital’s appointment scheduling system to the cloud can provide better scalability and data redundancy without altering the existing application’s core functionalities.
3. Refactoring
Refactoring focuses on restructuring and optimizing the existing codebase to improve performance, maintainability, and scalability. This method involves cleaning up the code, breaking down monolithic structures, and resolving technical debt while preserving the system’s external behavior.
This approach is particularly beneficial for healthcare systems that are difficult to maintain or have tightly coupled components. For example, refactoring a legacy patient management system can make it more adaptable to updates, easier to integrate with new tools, and more efficient in handling increased data loads.
4. Rebuilding
Rebuilding involves rewriting an entire application or system using modern technologies and architectures while retaining its essential business logic and core functionality. This method is ideal when the existing system is too outdated or costly to maintain or when a complete overhaul is necessary to meet new requirements.
For healthcare facilities, rebuilding may be the best option when dealing with legacy systems that cannot support critical new features such as telehealth integration or advanced analytics. A rebuilt system offers a fresh start, allowing the incorporation of the latest security protocols, compliance features, and improved user interfaces tailored to modern healthcare needs.
5. Replacing
Replacing a legacy system involves decommissioning outdated technology and implementing a new, modern solution that aligns with the organization’s long-term goals. This approach is often the most practical choice when the legacy system is beyond repair, or modernization is not cost-effective.
Healthcare organizations may replace older systems like outdated claims processing software with modern platforms offering better regulatory compliance, streamlined workflows, and enhanced automation capabilities. The new system can help reduce operational risks, improve data accuracy, and boost overall efficiency.
6. Rearchitecting
Rearchitecting involves redesigning the system’s architecture from outdated designs, such as monolithic structures, to modern architectures like microservices, cloud-native, or event-driven models. This method enhances scalability, flexibility, and maintainability, making adapting to evolving healthcare requirements easier.
Healthcare providers often choose rearchitecting to support modern needs such as cloud-native deployments or rapid feature delivery. A hospital information system can become more agile by shifting to a microservices architecture, allowing quicker updates and seamless integration with third-party healthcare applications.
Selecting the appropriate modernization method depends on the specific challenges and goals of the healthcare organization. Whether through encapsulation, rehosting, refactoring, rebuilding, replacing, or rearchitecting, modernizing legacy systems is a strategic investment in improving healthcare delivery and patient outcomes.
Step-by-Step Guide to Modernize Legacy Systems in Healthcare
Modernizing legacy systems in healthcare requires a structured approach to ensure success. Following a well-defined process helps healthcare organizations achieve improved efficiency, enhanced security, and better patient care outcomes. Here’s a step-by-step guide to effectively modernize legacy healthcare systems:
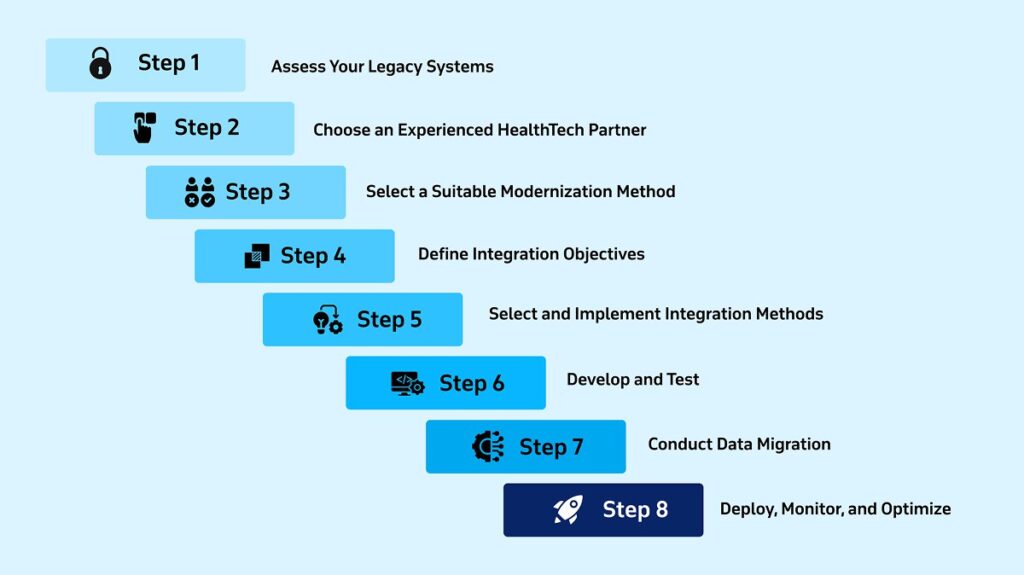
1. Assess Your Legacy Systems
The modernization journey begins with a comprehensive IT audit to evaluate all existing hardware, software, and systems. This involves analyzing current systems’ age, performance, compatibility, and security vulnerabilities. Engaging key stakeholders, including end-users, IT staff, and executive leadership, provides valuable insights into their expectations and needs for the updated system.
Financial implications are also a critical part of this assessment. Evaluating the total cost of ownership, including software maintenance, support, and downtime expenses, helps determine the long-term benefits of modernization. Based on this analysis, prioritize mission-critical systems that directly impact patient care, operational efficiency, and regulatory compliance. Developing a detailed report with findings, risks, and a phased modernization plan ensures a clear roadmap for the project.
2. Choose an Experienced HealthTech Partner
Selecting the right HealthTech partner is crucial for a successful modernization project. Look for a partner with a proven track record in healthcare technology, compliance expertise (e.g., HIPAA, HL7), and a deep understanding of clinical workflows. The ideal partner should offer end-to-end support, from initial assessment to implementation and ongoing maintenance.
A good HealthTech partner also brings expertise in emerging technologies like cloud computing, data integration, and cybersecurity. They should provide strategic guidance, help mitigate risks, and ensure that the modernization aligns with current and future organizational goals.
3. Select a Suitable Modernization Method
The choice of modernization method depends on the state of the legacy systems and the organization’s specific needs. Each method offers distinct advantages:
- Rehosting: Ideal for quickly migrating an application to the cloud without altering its code. It is a good fit when the existing application is stable and aims to leverage cloud infrastructure benefits like scalability and resilience.
- Refactoring: This involves restructuring the existing codebase to improve performance, maintainability, and compatibility without changing the application’s external behavior. This method is beneficial for reducing technical debt and enhancing long-term system reliability.
- Rearchitecting: Focuses on redesigning the application’s architecture, such as moving from a monolithic to a microservices architecture. This method enhances scalability, flexibility, and integration with modern technologies, although it requires more resources and effort.
- Rebuilding: This entails creating an entirely new application using modern technologies while retaining the core functionality of the old system. This approach is best when the legacy system is too outdated or costly to maintain, offering a fresh start with advanced features and improved performance.
- Replacing: This involves decommissioning the old system and adopting a completely new solution. This option is suitable when the legacy system no longer meets the organization’s needs and when starting fresh offers better alignment with strategic goals.
When deciding on a modernization approach, consider feasibility, cost, and the potential impact on clinical workflows. Ensure the team has the expertise for compliance, clinical data management, and technology integration.
4. Define Integration Objectives
Clear integration goals are essential for a successful modernization project. Determine whether the focus is improving data flow, adding new functionalities, or enhancing compliance with advanced technologies. These objectives should align with the organization’s strategic goals to ensure the modernization effort supports broader business success.
A robust data backup and recovery plan is also vital. Implementing cloud-based backup solutions can improve accessibility and security, helping maintain uninterrupted healthcare services even during system failures or data breaches. Regularly test the recovery process to ensure effectiveness and minimize potential data loss.
5. Select and Implement Integration Methods
Integration methods connect legacy systems with new applications, ensuring seamless data exchange and interoperability. Healthcare organizations can choose from the following:
- Enterprise Service Bus (ESB): Acts as a communication backbone, allowing multiple systems and applications to connect and share data effectively. ESB is beneficial in large healthcare organizations with complex IT environments.
- Point-to-Point Integration (P2P): Creates direct connections between two systems, offering a straightforward solution for simple integrations. While it is quick to implement, P2P can become challenging to manage as the number of systems grows.
- API Integration: Utilizes Application Programming Interfaces (APIs) to enable data exchange between software applications. This method is ideal for creating modular, scalable systems that support future upgrades and integration needs.
- Robotic Process Automation (RPA): Automates repetitive tasks, helping to bridge integration gaps in legacy systems with limited integration capabilities. RPA can be particularly useful in automating administrative tasks in healthcare facilities.
- Integration Platform as a Service (iPaaS): Provides cloud-based integration tools that streamline the connection between various applications and systems. iPaaS is an excellent choice for organizations looking to reduce infrastructure costs while achieving rapid integration.
Implementing these integration methods involves assessing existing systems, configuring middleware, defining data mappings, and ensuring robust security measures. Regular testing and user training are critical for a successful rollout.
6. Develop and Test
Developing and testing the modernized system involves a meticulous approach to ensure high-quality outcomes. Key steps include:
- Defining Requirements: Gather input from healthcare professionals, IT experts, and other stakeholders to establish precise system requirements.
- Iterative Development: Build and test the system in small increments to identify and resolve issues early.
- Cross-Functional Teams: Engage developers, quality assurance specialists, and subject matter experts to enhance collaboration and problem-solving.
- Comprehensive Testing: Perform usability, performance, security, and integration tests to validate the system’s functionality and ensure it meets healthcare standards.
Ensuring the system is intuitive, secure, and integrates well with existing healthcare infrastructure is critical for smooth adoption and optimal performance.
7. Conduct Data Migration
Data migration is a critical step in modernizing legacy systems. Start by cleaning and profiling legacy data to eliminate inconsistencies and errors. Define new data models and schemas to align with the modernized system’s architecture.
Execute the data migration using the Extract, Transform, and Load (ETL) process, ensuring data integrity and accuracy. Continuous testing during and after migration helps identify discrepancies and maintain data quality. Keeping stakeholders informed throughout the process ensures alignment and addresses concerns proactively.
8. Deploy, Monitor, and Optimize
The deployment phase involves launching the modernized system into the healthcare environment with minimal disruption to ongoing operations. Effective deployment requires robust monitoring tools like Splunk, Nagios, or SolarWinds to track system performance, detect issues early, and maintain system stability. Automated alerts help promptly identify performance anomalies, security threats, or system failures.
Regular performance analysis is crucial to fine-tuning processes, enhancing efficiency, and ensuring the system remains aligned with evolving healthcare requirements. Continuous optimization keeps the system running smoothly, supports high-quality patient care, and enables healthcare providers to adapt quickly to changes in the healthcare landscape.
When transitioning from outdated systems, an incremental approach to modernization is essential. KMS Healthcare specializes in integrating legacy healthcare platforms with modern cloud-based solutions, ensuring a smooth transition while minimizing disruptions. With a focus on backlog acceleration and operational continuity, KMS Healthcare helps organizations modernize effectively while maintaining service excellence.
FAQs
1. Why do businesses avoid upgrading a legacy system in healthcare?
Many healthcare organizations avoid upgrading legacy systems due to several challenges. Complex transitions can disrupt operations, and limited resources or expertise may hinder effective upgrades. Data migration poses risks of loss or corruption, while resistance to change from staff can slow progress. Some organizations are satisfied with existing systems and do not need an upgrade. Additionally, navigating new compliance and security requirements can add complexity to the modernization process. Despite these concerns, staying on outdated systems may lead to higher long-term costs, security risks, and missed opportunities for improved patient care.
2. How can you tell when it’s time to modernize your legacy systems?
You can tell it’s time to modernize your legacy systems when you notice signs like performance slowdowns, frequent security breaches, and poor user experience. High costs, limited functionality, and lack of vendor support also indicate a need for an upgrade. If your system struggles with device compatibility, integration limitations, or maintaining efficient workflows, modernization can help. Additionally, signs such as increased maintenance costs, system malfunctions, and difficulty adapting to new requirements highlight that your current technology may no longer meet your healthcare organization’s evolving needs.
Modernize Your Legacy Systems with KMS Healthcare
Upgrading legacy healthcare systems is a strategic move that enhances efficiency, strengthens security, and ensures compliance with evolving healthcare standards. An incremental approach to modernization minimizes disruptions and aligns with your organization’s long-term goals.
At KMS Healthcare, our Backlog Acceleration service offers a streamlined path to modernizing legacy systems without overwhelming your internal teams. We help reduce development backlogs, seamlessly integrate modern solutions, and maintain operational continuity throughout the transformation process.
Why Choose KMS Healthcare?
- Rapid Modernization: Experienced healthcare developers integrate quickly, reducing backlogs and advancing modernization projects.
- Independent, Efficient Execution: Our teams operate autonomously, allowing your staff to focus on core tasks without constant oversight.
- Flexible Scaling: Access on-demand expertise without the costs and challenges of hiring new staff.
Transform your legacy systems into future-ready healthcare solutions with KMS Healthcare. Contact us today.
