EMR (Electronic Medical Record) Data Integration stands as a cornerstone for advancing patient care quality and operational efficiency. Distinct from EHR (Electronic Health Record) integration, which encompasses a broader scope of health information, EMR data integration focuses on the seamless amalgamation of patient records within a single healthcare provider’s system. This guide dives deep into the methodologies and frameworks essential for achieving successful EMR data integration.
Understanding Electronic Medical Record (EMR) Data Integration
The healthcare industry is rapidly prioritizing EMR integration to enhance operational efficiency and healthcare data storage for healthcare providers and patients alike. However, the integration process may pose complexity and challenges, requiring specific knowledge and expertise.
What Is EMR Integration?
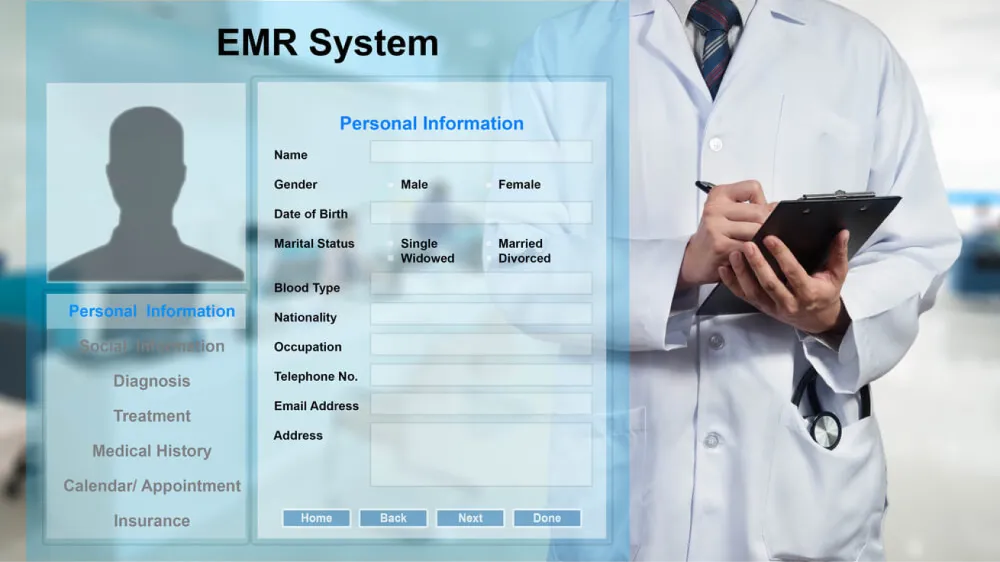
The Electronic Medical Record (EMR) is a digital alternative to traditional paper charts used by doctors to collect patient data. These records include vital information such as demographics, vital signs, medications, allergies, immunizations, lab results, and radiology reports.
EMR system integration is the connection between the organizations’ digital systems and other healthcare software applications to facilitate data sharing across clinical platforms. This process enables physicians to electronically document patient encounters and internal systems to generate clinical decision-support alerts based on best practices.
Overall, the goal of EMR data integration is to achieve interoperability for direct organizational impact. The integration will pave the way for effective communication and data exchange among diverse systems, regardless of the platform or language used.
The Importance of EMR Data Integration
Healthcare facilities manage and store extensive amounts of data for each patient visiting them. When this data is stored in paper charts or handwritten notes, sifting through it can be as daunting as finding a needle in a haystack.
Moreover, EMRs provide not only access to a patient’s medical record but also their medical information such as diagnosis, prescriptions, allergies, demographics, and even lab test results. In this case, EMR data integration is the only way to streamline these data digitally and open access to multiple health data systems.
The lack of proper integration networks connecting EMRs with other systems has also led to burnout among healthcare professionals, administrative staff, and patients. This burnout results from the inefficiencies of disparate systems and manual coordination among staff. Therefore, EMR data integration is crucial in ensuring a more resilient healthcare system that prioritizes the well-being of both healthcare providers and patients.
Benefits of EMR Integration
EMR integration offers valuable features that enhance efficiency and outcomes for all healthcare entities involved. The process not only improves healthcare operations, it enhances the patient experience, reflected by metrics such as:
- Enhanced data access
- Increased operational efficiency
- Boosted patient satisfaction
- Ensured healthcare data compliance

1. Enhanced Data Access
EMR system integration plays a critical role in enhancing data collection at the point of care across diverse healthcare systems and devices. By integrating EMRs, healthcare providers are empowered to access patient data anytime and anywhere throughout patient interactions, enabling them to deliver superior care. Enhanced coordination fosters more informed decision-making and facilitates a holistic approach to improving healthcare outcomes.
2. Increased Operational Efficiency
The integration of EMR systems streamlines clinical data transcription and eliminates the need for multiple entries across different systems – significantly reducing errors and minimizing the risk of manual data entry. Ideally, EMR integration allows healthcare professionals to spend less time on administrative tasks, giving them more time to prioritize patient care over paperwork.
3. Boosted Patient Satisfaction
EMR data integration gives an end to the repetitive tasks of patients, in which they have to recount their medical history or undergo redundant tests when seeing different clinicians. This integration enables healthcare providers to store, track, and access patient information easily, hence creating a personalized and efficient experience that enhances patient satisfaction.
Specific EMR integrations offer online scheduling and payment portals, along with features like reminders and feedback options to help reduce wait times and boost patient engagement.
4. Ensured Healthcare Data Compliance
Compliance with data protection regulations is of utmost importance, particularly in sectors handling sensitive personal information like healthcare. The integration of EMRs in this case plays a vital role in safeguarding patient data by effectively controlling access and limiting it to authorized personnel only. Therefore, EMR data integration assists healthcare organizations in maintaining compliance with industry standards, including HIPAA and HITRUST security standards.
Challenges Hindering EMR Integration Effectiveness
Despite the promising advantages of EMR integration, it also comes with various challenges. Therefore, healthcare organizations should recognize and tackle these barriers to optimize the implementation of EMR data integration. Some existing challenges include:
- Data standardization concerns
- Customization complexity
- Vendor lock-in

1. Data Standardization Concerns
Data standardization poses significant challenges for EMR integration due to formatting and mapping barriers. Varying data formats and terminologies among different EMR vendors hinder seamless data integration, making it hard to combine information from disparate systems effectively. And without standardized terminologies, such as SNOMED CT for diagnoses for example, the risk of data ambiguity and misinterpretation looms large.
Even when all systems are speaking the same language, mapping data elements between EMR systems remains complex and often necessitates custom mapping rules, leading to time-consuming processes and potential errors.
Moreover, it is crucial to maintain data integrity and quality. Inconsistent data entry in EMR systems can lead to errors, affecting the reliability of data analysis and patient care decisions.
Despite using a standardized language across EMR systems, the process of aligning data elements between different systems is intricate and typically requires tailored mapping rules. This complexity can result in protracted processes and the risk of errors. Furthermore, ensuring the accuracy and consistency of data entered into EMR systems is essential. Variations in how data is recorded can compromise the quality of data analysis and the dependability of decisions related to patient care.
2. Customization Complexity
EMR customization complexity arises from the diverse data structures and terminologies used by different vendors. As a result, tailoring integrations to align these variations into a unified format demands significant effort.
Besides, extracting specific data elements for integration may involve adapting processes for each EMR, leading to time-consuming tasks and requiring ongoing maintenance. Finally, integrating EMR data with other healthcare systems, for example, billing systems, also entails various adjustments in workflows, hence demanding more complicated customization to facilitate seamless data flow across various systems.
3. Vendor Lock-in
Vendor lock-in occurs when a company becomes excessively dependent on a particular vendor for products or services, making it difficult to switch to another vendor without substantial costs or disruptions.
To explain, being tied to one EMR vendor limits flexibility to choose the best solutions from various providers, therefore leading to the miss-out of innovation opportunities. Not to mention, data silos and interoperability issues might also occur due to proprietary formats and APIs, hence impacting data exchange and analysis.
Besides, data ownership and exportation issues may arise, with some vendors limiting access to data. This restriction can make transitions to other vendors or broader healthcare initiatives more complex. Also, a lack of negotiation power with a locked-in vendor may weaken the organization’s bargaining power with the vendors, leading to rising costs and hindering competitive pricing.
Strategies for Successful EMR Data Integration
To effectively address the aforementioned challenges and achieve successful EMR data integration, healthcare organizations should possess a comprehensive strategy from the outset. This strategy must adhere to five key steps:
- Planning and assessment for integration readiness
- Selecting the right integration tools and partners
- Building and testing EMR integration
- Ensuring compliance with regulatory standards
- Training and implementation

1. Planning and Assessment for Integration Readiness
The first step involves collecting and identifying specific needs and requirements for the integration, enabling a more precise Project Scope of Work (SOW) and optimized implementation budget.
Particularly, the integration project team should conduct a comprehensive analysis of business and technical conditions, including digital strategy and IT infrastructure, to identify any gaps in processes or technology.
Additionally, the discovery process before EMR integration should also include the investigation into various aspects such as data conversion, estimated time for EMR data integration, and procedures for accessing scanned images. Such engaging in meticulous planning will then allow the company to develop a comprehensive and well-informed strategy.
2. Selecting the Right Integration Tools and Partners
During the EMR data integration process, healthcare businesses encounter various challenges that necessitate expertise and cost-efficiency to minimize financial burden. To effectively manage and resolve these issues, engaging a reliable technology partner is crucial. The selection criteria for the right partner may vary based on specific company requirements, but a high-performing team should meet certain basic criteria. These include:
- Ensuring regulatory compliance of systems
- Providing cost-efficient software solutions
- Taking ownership of all technical project aspects
- Addressing hardware inconsistencies through suitable software architecture.
Besides, the selection of an appropriate EMR system is considered the foundation for seamless data exchange and interoperability. Therefore, businesses should consider EMR data integration tools that meet data standard compliance, interoperability levels, scalability, and cost requirements.
3. Building and Testing EMR Integration
During the EMR data integration process, adherence to interoperability standards is imperative to facilitate seamless data exchange within the medical organization. Clear data mapping strategies must be defined to align data structures, such as patient demographics, medical history, and prescriptions, between the systems.
Once the integration system is built, parallel integration testing and user acceptance testing should be conducted to promptly identify and resolve any issues. Additionally, implementing robust error-handling mechanisms is essential to effectively managing potential issues during the EMR integration process.
4. Ensuring Compliance with Regulatory Standards
Ensuring regulatory compliance with EMR software is crucial for hospitals to safeguard patient privacy, maintain data security, and adhere to industry standards.
To maintain this status quo, healthcare businesses should first familiarize themselves with relevant regulations and standards governing EMR software, such as HIPAA or HITRUST. Staying updated on changes to these regulations is also essential for ongoing compliance.
Regarding the implementation of data protection tactics, performing comprehensive audits of EMR software and related processes is also recommended. The process will include assessing security features, access controls, encryption capabilities, audit trail functionality and building backup systems. Prioritizing regulatory compliance not only protects patient data but also fosters trust among patients.
5. Training and Implementation
Proper training in EMR data integration is the key for healthcare staff and providers to effectively utilize technology and optimize workflows. The training should emphasize accurate handling of both internal and patient information, as well as other EMR interactions to reduce the risk of errors that could impact patient safety and operational quality.
EMR Data Integration Technologies
In addition to well-planned strategies, the healthcare industry can optimize its success by leveraging emerging technologies in EMR data integration. Particularly, standard protocols and solutions like HL7, cloud storage, and APIs play a vital role in this transformative process.

HL7 and FHIR Standards for Interoperability
The worldwide healthcare IT language, HL7, sets standards for collecting and exchanging medical information. HL7 FHIR, meanwhile, is tailored for web APIs, which can enhance interoperability. Regarding the growing complexity and volume of information in the US healthcare industry including data complexity, HL7 integration offers a solution by ensuring uniformity and bridging data exchange gaps. This standard supports various data formats, aiding in patient information management from admission to billing, therefore enhancing data exchange practices.
Cloud-Based Solutions for Scalable Integration
Cloud-based EMR solutions use cloud technology for secure storage, exchange, and protection of sensitive medical data. These systems enhance patient care, reinforce data security, and streamline healthcare operations. One key advantage is their scalability, which allows for accommodating growing healthcare data volumes without extra physical storage. Besides, cloud adoption cuts costs on infrastructure and expertise, aiding resource allocation efficiency to benefit both patients and healthcare providers.
FAQs
Are there specific standards or protocols used for EMR data integration?
EMR data integration relies on three key standards:
1. Health Level Seven (HL7): HL7 facilitates seamless sharing of patient data across different healthcare systems. It ensures interoperability and effective communication between disparate healthcare applications, enabling the exchange of critical information such as patient records, lab results, and medication data.
2. Fast Healthcare Interoperability Resources (FHIR): FHIR utilizes contemporary web technologies to enhance EMR integration. Its structured approach enables meaningful exchange of health information, promotes efficient integration, and provides comprehensive access to patient data in a patient-centric manner.
3. Clinical Document Architecture (CDA) is crucial for the efficient handling of clinical documents and seamless integration with EMR systems. CDA ensures structured clinical documents, enabling standardized sharing of patient data.
How can healthcare organizations ensure the security and privacy of integrated EMR data?
In order to comply with existing regulations such as HITECH and HIPAA, it is imperative for EMR to maintain stringent safety and security measures to prevent unauthorized access. Healthcare organizations can employ various strategies to bolster the security of their databases.
These include implementing robust user authentication protocols, ensuring regular data backups, utilizing firewalls, leveraging advanced encryption technologies, and incorporating secure browsing solutions.
How is EMR Integration Accomplished with Telehealth Systems?
The seamless integration of telehealth applications with EMR systems empowers healthcare providers to offer convenient remote care options for patients.
By eliminating the need to switch between multiple platforms, an integrated EMR provides a unified, single platform for streamlined coordination of remote care. This integration significantly enhances the speed and efficiency of care delivery, ultimately leading to improved patient outcomes.
How is EMR Integration Accomplished with Clinical Trial Management Systems?
The integration of an EMR with a Clinical Trial Management System (CTMS) offers significant advantages, primarily in the realm of billing. This seamless integration facilitates the streamlined processing of study billing definitions, enabling efficient transfer from the CTMS to the EMR. This integration holds immense potential for enhancing billing processes within clinical trials and research studies.
Level up Your EMR Data Integration Process With KMS Healthcare Now
Efficient budgeting and operations are vital components of EMR integration. Therefore, healthcare organizations must seek a trusted vendor to accompany them on this transformative journey.
With nearly 15 years of experience in healthcare and a proven track record of successfully delivering numerous healthtech projects, KMS Healthcare is the ideal partner you’ve been searching for. Our main focus is upgrading your EMR system to a higher standard through a well-rounded data integration strategy, enabling you to fully leverage all the benefits it offers.
Schedule a consultation with our experts now to build up your own strategies for compatible and scalable EMR integration right from today.

Reference
(n.d.). Is The Future Of Healthcare EMR Centered On Partner Ecosystems? Forbes. https://www.forbes.com/sites/davidchou/2024/01/29/is-the-future-of-healthcare-emr-centered-on-partner-ecosystems/?sh=5a990a415e8f
(n.d.). Clinical Trial Management System Definition. Institute of Translational Health Sciences. https://www.iths.org/ctms/about/what-is-a-clinical-trial-management-system/